2/13/2019, Journal of Feline Medicine and Surgery; Translation 10.2.2021
Original article: Efficacy and safety of the nucleoside analog GS-441524 for treatment of cats with naturally occurring feline infectious peritonitis
Niels C Pedersen, Michel Perron, Michael Bannasch, Elizabeth Montgomery, Eisuke Murakami, Molly Liepnieks, and Hongwei Liu
Abstract
Goals
The aim of this study was to determine the safety and efficacy of the nucleoside analog GS-441524 for cats suffering from various forms of naturally occurring feline infectious peritonitis (FIP).
Methods
Cats ranged in age from 3.4 to 73 months (mean 13.6 months); 26 cats had wet or mixed FIP, 5 dry form FIP. Cats with severe neurological and ocular FIP were not included in the study. The group started with GS-441524 at a dose of 2.0 mg / kg SC q24h for at least 12 weeks, which increased to 4.0 mg / kg SC q24h when indicated.
The results
Four of the 31 cats that had severe disease died or were euthanized within 2-5 days and the fifth cat after 26 days. The remaining 26 cats completed the planned 12 or more weeks of treatment. Eighteen of these 26 cats remain healthy at the time of publication (OnlineFirst, February 2019) after one round of treatment, while eight others suffered relapses within 3-84 days. Six of the relapses were non-neurological and two were neurological. Three of the eight rats were treated again with the same dose, while the five cats were increased from 2.0 to 4.0 mg / kg every 24 hours. Five cats treated with a second higher dose, including one with neurological disease, responded well and were healthy at the time of publication. However, one of the three cats re-treated with the original lower dose relapsed with neurological disease and was euthanized, while the two remaining cats responded favorably but a second relapse occurred. These two cats were successfully treated for the third time at a higher dose, which resulted in 25 long-term surviving cats. One of the 25 successfully treated cats was subsequently euthanized due to probable unrelated heart disease, while 24 remained healthy.
Conclusion and meaning
GS-441524 has been shown to be safe and effective in the treatment of FIP. The optimal dose was 4.0 mg / kg SC q24h for at least 12 weeks.
Keywords: Nucleoside analogue, GS-441524, feline infectious peritonitis, FIP, clinical study
Introduction
Drugs that inhibit viral replication have become a focal point in the treatment of human acute and chronic RNA and DNA infections. However, the development of interest in antiviral drugs for animal infections has been much slower. This is especially true for cats, which suffer from several chronic viral infections similar to humans. Infectious agents include feline leukemia and immunodeficiency virus (FeLV and FIV), feline herpesvirus (FHV), virulent systemic calicivirus, and coronavirus causing feline infectious peritonitis (FIPV). FeLV and FIV infections can be kept under control through testing, isolation and / or vaccination. The FHV-associated disease was the first feline viral infection to use an antiviral agent for treatment. Highly fatal systemic calicivirus affects only a small number of cats. FIPV infection is the best candidate for the development of antiviral drugs because vaccines are ineffective, the environment with many cats makes it very difficult to prevent and kills 0.3-1.4% cats worldwide.
The emergence of exotic diseases such as Ebola, Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) in humans has prompted intensive research into drugs that inhibit RNA replication. One of the most promising antiviral drugs for nascent RNA viruses is the prodrug adenosine nucleoside monophosphate GS-5734 (Remdesivir; Gilead Sciences). GS-5734 demonstrated efficacy in experimental Ebola in rhesus monkeys and inhibited both epidemic and zoonotic coronaviruses in tissue cultures and mouse infectious models. These promising findings initiated research into GS-5734 and its original nucleoside GS-441524 against FIPV infection in cats. GS-441524 and GS-5734 have comparable EC50 (1.0 μM) and CC50 (> 100 μM) values against FIPV in feline cells. Therefore, it was decided to focus on the less chemically complex GS-441524 for further testing with laboratory cats. A pharmacokinetic study in two laboratory cats showed sustained and effective plasma levels of GS-441524 over 24 hours after a dose administered subcutaneously (SC) or intravenously (IV). These results were extended to 10 laboratory cats with experimentally induced abdominal effusion feline infectious peritonitis (FIP). This study demonstrated that GS-441524 is highly effective against experimental FIP, paving the way for this clinical study.
The aim of this study was to demonstrate the safety and efficacy of GS-441524 in the treatment of cats with naturally occurring FIP. Small molecule drugs, such as GS-441524, weigh <900 daltons and are approximately 1 nm in size and can easily penetrate cells and interact with key target molecules. Unlike previously published substances or drugs that inhibit FIPV by inhibiting cellular processes by viruses used for their replication, small molecules such as GS-441524 interfere directly with virus-encoded replication processes.
Materials and methods
Preparation of the drug
GS-441524 was provided by Gilead Sciences as a pure and highly stable powder, which was diluted to a concentration of 10 or 15 mg / ml in 5% ethanol, 30% propylene glycol, 45% PEG 400, 20% water (pH 1.5 with HCl). The solution was placed in sterile 50 ml glass vials in which it was shaken until dissolved and then subjected to a sonic water bath for 5 to 20 minutes until clear. The diluted drug was refrigerated and used within 3-4 weeks.
Study concept
This study was conducted in accordance with Protocols 19336 and 19863, approved by the Institutional Committee on the Care and Use of Animals and the Clinical Trials Evaluation Committee of the Veterinary Teaching Hospital of the University of California, Davis. The institutional rules exclude the use of sick cats from shelters or similar establishments, due to the requirement of legal ownership / adoption and treatment under specific conditions with the consent of the owner (supplementary material). The study did not include a control group because there is no effective comparative treatment. The placebo group was not included either, as in vitro and in vivo preparatory studies indicated that GS-441524 would be safer and more effective than any treatment.
Case selection and diagnosis confirmation
Cats with FIP were received from owners or their veterinarians who were looking for current treatment options or access to a previous study of antiviral drugs. The initial diagnosis of FIP was based primarily on characteristic signaling, clinical history and symptoms of the disease, results of routine laboratory tests, and examination of abdominal or thoracic effusions. A more definitive diagnosis based on RT-PCR or immunohistochemistry was desirable, but not a prerequisite for inclusion. Cats with overt ocular or neurological disease were excluded due to doubts about the ability of antiviral drugs, including GS-441524, to cross the blood-brain or blood-eye barrier.
31 cats and their owners were admitted to the study (Table 1). Owners or representatives of 26 cats came for initial treatment directly to UC Davis and five owners and their cats (CT59, CT73, CT76, CT78, CT80) were treated by a local veterinarian. The cats present at UC Davis were re-evaluated, their FIP diagnosis was re-confirmed on the basis of signaling, clinical history, physical examination, results of previous laboratory tests and complete blood count (CBC), serum protein and effusion analyzes. Thoracic or abdominal effusion in cats with wet FIP was confirmed positive for FIPV 7b RNA by RT-PCR. Cats with signs of non-fusion FIP were further tested by abdominal and thoracic ultrasonography for primary lesions. The eye disease was confirmed by the VMTH Ophthalmology Service, UC Davis. The neurological condition in cases with possible symptoms of central nervous system disease was evaluated by the VMTH neurological service.
Table 1
List of 31 cats included in the test, including laboratory designation, cat name, breed, clinical form of infectious peritonitis (FIP) and date of diagnosis
| ID | Name | Date of birth | Tribe | Gender | Origin | Date of diagnosis | FIP form |
|---|---|---|---|---|---|---|---|
| CT52 | Moon | 9.1.2017 | Savannah | F | Breeder | 24.4.2017 | Abdominal effusion |
| CT53 | Ice Bear | 2.8.2016 | DLH | MC | Rescue team | 5.5.2017 | Abdominal effusion |
| CT54 | Charolett | 11.7.2016 | Siberian | F | Breeder | 15.4.2017 | Abdominal effusion |
| CT55 | Dempsey | 26.6.2016 | DSH | MC | Rescue team | 15.4.2017 | Abdominal effusion |
| CT56 | Mudsa | 1.7.2016 | DSH | MC | Shelter | 12.5.2017 | Abdominal effusion |
| CT57 | Boone | 31.10.2016 | DSH | FS | Rescue team | 8.5.2017 | Abdominal effusion |
| CT58 | Justyna | 17.4.2016 | Ragdoll | F | Breeder | 25.5.2017 | Abdominal effusion |
| CT59 | Bubba | 11.4.2011 | DLH | MC | Wandering | 10.4.2017 | Abdominal non-fusion |
| CT60 | Joey | 25.7.2016 | DSH | MC | Rescue team | 20.5.2017 | Abdominal effusion |
| CT61 | Hudson | 1.7.2016 | DSH | MC | Rescue team | 29.5.2017 | Thoracic effusion |
| CT62 | Luca | 10.3.2016 | DSH | MC | Rescue team | 30.5.2017 | Abdominal effusion |
| CT63 | Bao Bao | 6.11.2016 | DSH | MC | Rescue team | 3.6.2017 | Abdominal effusion |
| CT64 | Cedrick | 27.6.2016 | DSH | MC | Rescue team | 22.5.2017 | Abdominal non-fusion |
| CT65 | Mona | 14.3.2016 | Exotic SH / Persian | F | Breeder | 11.6.2017 | Thoracic effusion |
| CT66 | Squeekers | 7.6.2016 | DSH | FS | Shelter | 14.6.2017 | Abdominal effusion |
| CT67 | Double | 2.3.2016 | Ragdoll | FS | Breeder | 20.6.2017 | Abdominal effusion |
| CT68 | Tuckerman | 8.5.2016 | Maine Coon | MC | Rescue team | 22.6.2017 | Abdominal effusion |
| CT69 | Danny | 16.6.2015 | Snowshoe | MC | Shelter | 22.6.2017 | Thoracic effusion |
| CT70 | Tolstoy | 1.8.2014 | DSH | MC | Rescue team | 25.6.2017 | Abdominal effusion |
| CT71 | Amadeus | 29.6.2016 | DSH | MC | Wandering | 20.6.2017 | Thoracic effusion |
| CT72 | Bella | 25.2.2017 | British SH | F | Breeder | 20.6.2017 | Abdominal effusion |
| CT73 | Siersha | 8.8.2015 | DSH | FS | Shelter | 21.6.2017 | Abdominal non-fusion |
| CT74 | Maive | 4.3.2017 | Siberian | FS | Breeder | 7.7.2017 | Abdominal effusion |
| CT75 | Lucy | 31.3.2017 | DSH | F | Rescue team | 10.7.2017 | Abdominal effusion |
| CT76 | Pie | 20.7.2016 | Exotic SH | M | Breeder | 28.6.2017 | Abdominal effusion |
| CT77 | Mila | 15.3.2017 | Siberian | FS | Breeder | 3.7.2017 | Abdominal effusion |
| CT78 | Polly | 1.3.2016 | DSH | MC | Rescue team | 22.7.2017 | Abdominal non-fusion |
| CT79 | Oona | 21.9.2016 | Himalayan | F | Breeder | 18.7.2017 | Chest non-fusion |
| CT80 | Fezzik | 17.10.2016 | DLH | MC | Wandering | 25.7.2017 | Abdominal effusion |
| CT81 | Jewelkat | 8.9.2016 | Persian | FS | Breeder | 1.8.2017 | Thoracic effusion |
| CT82 | Tiko | 8.4.2016 | DSH | MC | Rescue team | 6.8.2017 | Abdominal effusion |
Treatment regimen
Based on previous tissue culture experiments and pharmacokinetic studies in laboratory cats, the initial dosing regimen for GS-441524 was set at 2.0 mg / kg SC q24h. Based on experience with the 3CL protease inhibitor GC376 against naturally occurring FIP, a minimum treatment period of 12 weeks was established. Treatment was extended by one or more weeks in cats that still had abnormal serum protein levels. In later stages of the study, the dose was increased from 2.0 to 4.0 mg / kg in cases where treatment had to be prolonged or when the disease had relapsed. Every 4 weeks, a new dose of 1 or 3 ml Luer lock syringes with 1 inch Luer 22G (0.7x25mm) Luer needles was sent to the owners. The syringes were stored in a refrigerator and warmed to room temperature before administration. Injections were given along the spine from 2 cm behind the shoulder blades to half of the lumbar region and halfway down to the adjacent chest and hips.
Monitoring during the initial treatment period
At the time of entry into testing, the cats had stopped all treatment that was not necessary - antibiotics, corticosteroids, interferons, pentoxifylline, non-steroidal anti-inflammatory drugs, or painkillers. During their stay at UC Davis, cats were monitored every 12 hours for temperature, appetite, activity, urination and defecation. Blood was collected at 1-3 day intervals to evaluate hematocrit, total protein, bilirubin, white blood cell count and differential white blood cell count.
Ascites samples were taken initially and then taken at one or more daily intervals for as long as possible and tested for FIPV 7b RNA transcript levels by quantitative (q) RT-PCR (IDEXX molecular diagnostics). Formalin-fixed tissue sections from five dissected cats were subjected to immunohistochemistry for FIPV nucleocapsid protein.
Monitoring of initial and long-term response to treatment
Cats were released for home treatment when a significant favorable response to treatment was noted, usually within 3-5 days. During this period, owners were instructed on the proper administration of subcutaneous injections and were encouraged to continue daily records of body temperature, activity, appetite, defecation and urination, and weekly body weight measurements. CBC and serum chemical panel were performed at monthly intervals by local veterinarians or during VMTH visits. Any abnormal symptoms or behaviors should be recorded and reported immediately. Reasonable euthanasia was usually performed by the owner's veterinarian or, if possible, at UC Davis. The bodies were immediately cooled and sealed in plastic bags, and sent within 2 or fewer days in ice-cooled containers to UC Davis by express mail. Autopsies were performed by one of the authors (ML) at the Anatomic Pathology Service, School of Veterinary Medicine, UC Davis. The owner's request for the final disposition of the body was respected.
The results
Disease signaling and presentation
The study included 31 cats aged 3.4 to 73 months (mean 13.6 months) (Table 1). Eighteen cats were domestic short-haired and long-haired, 13 cats represented representatives of 10 different breeds (Table 1). Domestic cats were adopted from cat rescue organizations (n = 13), shelters (n = 2) or stray cats from the area (n = 3). The study included 14 females (7 neutered; 7 neutered) and 17 males (1 neutered; 16 neutered).
Twenty-six of the 31 cats had wet FIP (6 thoracic, 20 abdominal). Five cats had non-fusion FIP; four of them (CT59, CT64, CT73, CT78) with disease located in the abdomen (mesenteric and ileo / cecal / colic lymph nodes) and one (CT79) in the chest (lungs, hilar lymph nodes) (Table 1). Four additional cats showed signs of earlier dry FIP, which turned into an effusion form (CT57, CT65, CT67, CT71) (Table 1). Gross symptoms of eye disease corresponding to FIP were confirmed by ophthalmoscopic examination in three of the 31 cats (CT56, CT65, CT71). Two cats (CT71, CT80) reluctantly or were unable to jump to elevated sites at all, indicating neurological impairment.
Treatment results
Four cats were euthanized (CT62, CT72, CT75) or died (CT56) during the first 2-5 days due to serious illness and other complications, and the fifth cat was euthanized (CT54) after 26 days due to lack of response to treatment (Figure 1). Treatment was uninterrupted, with the exception of three cats who were given a two-week rest period at week 4 (cat CT80) or week 8 (cat CT53, CT71) due to injection problems and skin reactions (Figure 1). After the second relapse, the CT53 cat was treated for 8 and not 12 weeks due to an increase in blood urea and an increase in serum levels of symmetric dimethylarginine (SDMA).

Treatment time scale and clinical outcome of 31 cats enrolled in clinical study GS-441524. The treatment period is indicated by a solid line (dose 2 mg / kg) or a dashed line (dose 4 mg / kg). Asterisks indicate a relapse point. The end date of treatment for cats that have achieved permanent clinical remission is indicated in parentheses. The time point and cause of death are marked with a cross
The clinical response of the 26 cats that completed at least 12 weeks of treatment was dramatic. The fever usually resolved within 12-36 hours (Figure 2), along with a significant increase in appetite, activity levels, and weight gain on a daily basis. Abdominal effusions quickly disappeared within 1-2 weeks, starting at about 10-14. the day after starting treatment. Cats with thoracic effusions, usually showing shortness of breath, were sucked out by practical private veterinarians before the pleural effusions were aspirated before arriving at UC Davis. Residual shortness of breath and thoracic effusion responded quickly to treatment and were no longer visible at all after 7 days. Jaundice resolved slowly over 2–4 weeks, with a decrease in hyperbilirubinemia. Signs of eye disease began to disappear within 24-48 hours and ceased to be apparent on the outside even for ophthalmoscopic examination within 7-14 days. Enlarged mesenteric and ileo / cecal / colic lymph nodes began to shrink during treatment. According to the owners' estimates, all 26 cats looked normal or almost normal on the outside after 2 weeks of treatment. After 2 weeks of treatment, the emphasis was on monitoring several blood test parameters. Key values included hematocrit, total white blood cell count, absolute lymphocyte count, total serum protein, serum globulin, serum albumin, and albumin: globulin ratio (A: G).

Mean (solid line) and 1 SD (standard deviation) (dashed) body temperatures during the first 5 days of GS-441524 treatment. The normal temperature range for cats is 37.7-39.1 ° C (100-102.5 ° F). Temperatures dropped to the normal range within 12-36 hours of treatment
Eighteen of the 26 cats that received at least 12 weeks of uninterrupted primary treatment required no further treatment. However, eight other cats suffered disease relapses within 3–84 days (mean 23 days) (Figure 1). This group included three cats that temporarily discontinued initial treatment (CT53, CT71, CT80), and five cats (CT53, CT57, CT60, CT68, CT73) that required extended primary treatment (Figure 1). The disease relapses in 2/8 cats (CT57, CT71) were apparently neurological in nature with high fever and strong posterior ataxia and incoordination, while the disease relapses in the remaining six cats consisted mainly of fever, anorexia and decreased activity. Only one cat (CT60) had an obvious abdominal discharge during the relapse. One cat (CT57) was euthanized 2 weeks after relapse with neurological symptoms that did not respond to the second round of treatment.
In eight cats, it was decided to increase the dose of GS-441524 from 2.0 to 4.0 mg / kg, either due to prolongation of treatment (CT77, CT80) or due to one (CT60, CT68, CT71, CT73) or two relapses ( CT53, CT63), or because the relapse had a neurological form (CT71). All eight cats responded positively to the booster regimen.
A total of 25/26 cats treated for 12 weeks or more achieved permanent remission of FIP, although one subsequently died of an unrelated heart problem (see "Autopsy Findings"). The longest surviving cats at the time of publication (OnlineFirst, February 2019) stopped treatment in August 2017 and the shortest in May 2018, all after the end of the observation period, in which relapse could still occur (ie 84 days after the end of treatment). The 24 surviving cats will be carefully monitored for recurrence of symptoms and will be regularly tested for total protein, globulin, albumin and A: G ratios during the first year. Less intensive monitoring will be performed for the rest of the cats' lives. Owners were advised to avoid unnecessary strain on cats during the first 3 months, even though four cats (CT52, CT58, CT65, CT79) and one cat (CT76) underwent trouble-free castration.
Indicators of favorable response to treatment
The simplest long-term measure of treatment effectiveness was body weight. Weight gain of 20–120% occurred during and after treatment, even in cats that were 1 year or older at the time of diagnosis. Significant growth also appeared in younger cats, as their owners independently noted. These significant post-treatment growth accelerations suggested that FIP was subclinical in many cats for some time before diagnosis and affected their growth. CBC (hematology) and chemical profile (biochemistry) have also been shown to monitor the later effects of treatment and to observe possible drug toxicities.
CBCs (Hematology)
Cats showed an increased white blood cell count, which fell to normal during the first 2 weeks of treatment (Figure 3a). Lymphopenia recorded at the time of admission disappeared during the first week of treatment (Figure 3b). Mild to moderate anemia was observed on admission, resulting in hematocrit (PCV) (Figure 4). Hematocrit did not return to normal until 6-8 weeks of treatment. Absolute total white blood cell and lymphocyte counts were the only significant values during the first week of treatment, while PCV provided a more accurate picture of the course of treatment during the first 8 weeks.
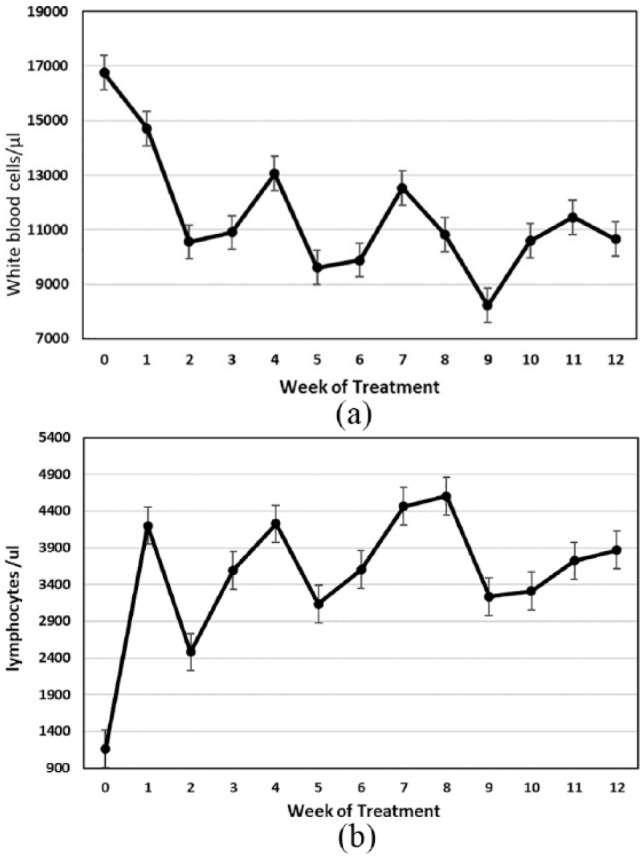
(a) Mean standard deviation white blood cell count in 26 cats that completed a primary treatment regimen for 12 weeks or more. (b) Mean absolute lymphocyte count in blood with standard deviation in 26 cats that had completed at least 12 weeks of treatment

Hematocrit (PCV) with a standard deviation for 26 cats that have completed at least 12 weeks of treatment. The dotted line indicates the growth trend of PCV over time
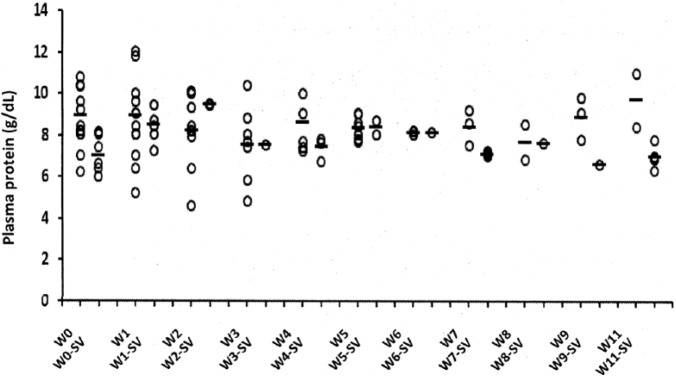
Serum protein changes
Cats with FIP often showed higher than normal total serum protein levels, high serum globulin levels, low serum albumin levels, and low A: G ratios (Figures 5-7). Serum protein abnormalities progressively improved and reached normal values after 8-10 weeks of treatment (Figures 5-7). Total protein levels were the least informative, indicating a low R2 (0.1883) trend line (Figure 5). However, 3 weeks after the start of treatment, there was a dramatic and transient increase in total protein levels (Figure 5). This phenomenon was related to an increase in serum globulins (Figure 6a) at a time of rapid regression of abdominal effusions.

Mean serum total protein levels and standard deviation for 26 cats that have completed at least 12 weeks of treatment

(a) Mean serum globulin levels and standard deviation for 26 cats that have completed at least 12 weeks of treatment. (b) Mean serum albumin levels and standard deviation for 26 cats that have completed at least 12 weeks of treatment

Mean albumin: globulin (A / G) ratios and standard deviation for 26 cats that have completed at least 12 weeks of treatment
Plasma globulin levels increased during the first 3 weeks of treatment, peaked and then slowly decreased to a maximum reference value of 4.5 g / dl or less by week 9 (Figure 6a). Although globulin levels appear to reflect treatment status over time, a low R2 (0.3621) indicated that this was a less reliable indicator of treatment progress.
Serum albumin levels of 26 cats treated for at least 12 weeks were usually low (⩽3.2 g / dl) at the time of treatment (Figure 6b). Albumin levels then increased slowly and reached normal levels after 8 weeks. The trend line for this increase in albumin was high R2 (0.79), making serum albumin levels as well as PCV a good indicator of treatment progress. As expected, the A: G ratio showed an equally strong trend line over time and around the 8th week of treatment the level exceeded 0.70 (Figure 7).
Decreased viral RNA levels in ascitic fluid cells in association with treatment
During the first 2-9 days of antiviral treatment, sequential ascites samples were taken from eight cats and tested for viral RNA levels by qRT-PCR (Table 2). The most reliable source of FIPV RNA was whole effluents or their cell fractions. In 7/8 cats, viral RNA levels dropped within 2-5 days, often to undetectable levels. One cat (CT54) did not show a significant decrease in viral RNA levels within 9 days.
Table 2
Levels of feline infectious peritonitis 7b RNA transcription in whole ascites or ascitic fluid cell fraction during initial treatment GS-441524
| Sample ID | Treatment days | Sample type | Copies of viral RNA / ml |
|---|---|---|---|
| CT52 | 0 | Ascites | 9.44 × 104 |
| 3 | Ascites | Undetectable | |
| CT54 | 0 | Ascites | 8.49 × 105 |
| 2 | Ascites | 6.97 × 104 | |
| 4 | Ascites | 2.44 × 103 | |
| 7 | Ascites | 2.07 × 103 | |
| 9 | Ascites | 6.46 × 104 | |
| CT62 | 0 | Ascites | 5.96 × 103 |
| 2 | Ascites | 1.53 × 103 | |
| 8 | Ascites | Undetectable | |
| CT74 | 0 | Cells | 6.51 × 106 |
| 2 | Cells | 3.39 × 105 | |
| CT75 | 0 | Cells | 9.08 × 106 |
| 3 | Cells | 4.75 × 105 | |
| 4 | Cells | 2.50 × 105 | |
| CT77 | 0 | Ascites | 5.47 × 104 |
| 2 | Ascites | 3.93 × 103 | |
| CT80 | 0 | Ascites | 4.10 × 103 |
| 2 | Ascites | Undetectable | |
| CT82 | 0 | Ascites | 1.13 × 104 |
| 5 | Ascites | Undetectable |
Side effects observed during and after treatment
Limited injection site reactions. Two types of injection site reactions have been observed and it has not been established whether they were due to the drug, the diluent or both. Immediate responses to pain were manifested by vocalization, occasional growling, and postural changes lasting 30-60 seconds. These initial reactions eased over time as owners became more skilled at injecting and cats gradually adapted to this routine. Sixteen of the 26 cats treated experienced injection site reactions (Table 3). Reactions were most common during the first 4 weeks and progressed to open wounds in only 7/16 cats. Ulcerations healed within 2 weeks by trimming the surrounding hair and gently cleaning the wound with a cotton swab soaked in one part household hydrogen peroxide and two parts water twice a day. Only three cats had noticeable scars at the injection sites.
Table 3
Injection site reactions in 16 of 26 cats treated with GS-441524 for 12 weeks or more
| Cat ID | Superficial lesions | Open wounds | Scars |
|---|---|---|---|
| CT53 | 3 | 1 | 0 |
| CT58 | 1 | 0 | 0 |
| CT60 | 0 | 0 | 2 |
| CT61 | 5 | 0 | 0 |
| CT63 | 2 | 2 | 0 |
| CT64 | 1 | 0 | 1 |
| CT65 | 9 | 1 | 1 |
| CT66 | 3 | 2 | 0 |
| CT68 | 4 | 0 | 0 |
| CT71 | 5 | 1 | 0 |
| CT73 | 7 | 1 | 0 |
| CT74 | 3 | 1 | 0 |
| CT76 | 10 | 0 | 0 |
| CT78 | 7 | 0 | 0 |
| CT79 | 2 | 0 | 0 |
| CT82 | 2 | 0 | 0 |
Systemic drug reactions. GS-441524 treatment was remarkably safe for a total of 12-30 weeks. No long-term abnormalities were observed in CBC values (Figures 3 and 4). Liver and kidney function tests and amylase / lipase levels remained normal during and after treatment (Supplemental Figures S1 - S3). The only exception was the CT53 cat, which had a progressive increase in blood urea (BUN) to 35 mg / dl (reference interval [RI] 16–37 /g / dl) and a sudden increase in SDMA (20 µg / dl) (RI 0- 14 /g / dl) after 8 weeks in the third round of treatment in a 4 mg / kg booster regimen. Although these symptoms were still mild in nature, it was decided to discontinue treatment. These abnormalities were no longer present when tested 1 month later and the cat is currently in remission.
Autopsy findings
Four cats (CT56, CT62, CT72, CT75) were euthanized or died within 2-5 days of study entry, and necropsies were performed on all but the CT75 cat. The fifth cat (CT54 cat) was euthanized after 26 days of treatment. All five of these cats had severe abdominal effusion disease. At CT54 and CT56, necropsy revealed evidence of extensive pyogranulomatous vasculitis involving the abdominal viscera, central nervous system, and eyes. In the CT56 cat, the ileal wall was also compromised in the area of dense infiltrate and secondary bacterial sepsis. The CT72 cat had severe abdominal pyogranulomatous vasculitis with moderate to severe peripheral edema and adrenal cortex mineralization. The CT62 cat suffered from severe pyogranulomatous and fibrinosuppurative peritonitis, which was complicated by acute gastric perforation associated with plant material and intralesional bacteria suggestive of sepsis. The CT75 cat exhibited a chronic form of FIP characterized by severe growth retardation, massively low protein / low cell effusion, accelerated cardiac function suggestive of impaired cardiac function, and moderate peripheral edema. The echocardiogram showed bilateral atrial enlargement, but no sign of primary heart disease. The cat appeared to respond to GS-441524 and was released. The cat fell into shock 2 days later and was euthanized without autopsy.
At the time of necropsy of CT56, CT72 and CT75 cats, no FIPV virus was detected using qRT-PCR, although pre-treatment ascites samples were positive. Cat ascites CT54 showed a positive qRT-PCR result throughout treatment (Table 2) and the tissues were still immunohistochemically positive at the time of necropsy.
After successfully completing one or more rounds of treatment, two more cats were euthanized. The CT57 cat was normal after one round of treatment, but relapsed with severe neurological symptoms 2 weeks later. The cat did not respond to re-treatment and was killed. Lesions typical of FIP were found in the brain and abdomen, but were negative for FIPV determined by immunohistochemistry for nucleocapsid protein or for 7b RNA by qRT-PCR. The CT80 cat was successfully treated for effusive abdominal FIP, but 4 weeks later she developed severe hind leg and lower back pain. The cat was found to have a marked thickening of the left ventricular wall and septum, which caused severe ventricular narrowing (Figure 8). The microscopic appearance of the left ventricular wall was typical of congenital feline hypertrophic cardiomyopathy (HCM). No gross or microscopic FIP lesions were detected in the abdomen, chest, eyes, brain or spine, and neither FIPV nor FIPV RNA was detected by qRT-PCR.

CT80 cat's heart section showing extreme left ventricular and septal wall hypertrophy and extreme ventricular narrowing
Discussion
GS-441524 is the second targeted antiviral drug tested for the treatment of FIP in the last 2-3 years after GC376. The two drugs inhibit viral replication in two very different ways, either by terminating viral RNA transcription or by blocking the cleavage of the viral polyprotein. Both processes are a well-known target for the treatment of some human viral diseases. A key issue is to compare nucleoside analogue treatment with viral protease inhibitor therapy. The two drugs gave virtually identical results in tissue culture studies and experimentally infected cats. However, the efficacy against naturally occurring FIP appeared to be higher with GS-441524 than with GC376. Six of the 20 cats treated with GC376 remain in remission to this day (Pedersen NC, unpublished data, 2018) compared to 25/31 cats treated with GS-441524. Diseases that did not respond to re-treatment occurred in 14/20 cats with GC376 but only in one cat treated with GS-441524. 8 of the 14 GC376-associated relapses were neurological, compared to 2/8 GS-441524 relapses. One of the two neurological relapses in cats treated with GS-441524 responded to re-treatment with a higher dose, whereas neurological relapses with GC376, even at an increased dose, were no longer treatable. Both treatments caused similar injection site reactions. Both drugs appear to be relatively safe, although GC376 interfered with the development of permanent teeth when given to younger kittens.
Although the results of the clinical study appear to favor GS-441524, some differences may have been affected by the way the two drugs were administered. The effectiveness of GC376 could be improved if all 20 cats were treated without interruption for 12 weeks, instead of being treated progressively over longer periods starting at only 2 weeks. Five of the six cats treated with GC376 were among the seven cats that were treated continuously for 12 weeks, while only one of the 13 cats treated once or more was treated for a shorter period of time. These shorter durations of treatment were necessary to determine the 12-week period used for all cats in this study. In addition, the GC376 clinical trial included fewer cats and was limited by limited drug delivery, making it difficult to test other dosing regimens. Therefore, GC376 should be further studied prior to any final comparison using a minimum of 12 weeks with a higher dose and more cats. It would also be important to evaluate both types of drugs in combination at some point in the future, as is the case with HIV / AIDS and hepatitis C.
Premature deaths should be considered in any study of this type, but how should they be considered in an efficacy analysis? Five premature deaths in this study were included in the GS-441524 efficacy analysis, but were excluded in study GC376. It is important to determine the status of the virus at the time of death to include deaths in the study. Viral RNA was not detected in three necropsed cats that died after 2-5 days of treatment with GS-441524, indicating that the drug was effective but the disease was at an advanced stage. This was not the case for the fourth dissected cat, which survived 26 days; viral RNA levels did not decrease throughout the treatment period and the symptoms of the disease did not improve. Therefore, it is possible that this cat died as a result of an unsuccessful cessation of virus replication. Resistance to GS-5734 (Remdesivir), a prodrug of GS-441524, has been associated with amino acid mutations in RNA polymerase and corrective exonuclease in tissue culture propagated coronaviruses. Whether this cat has developed similar resistance remains to be determined. Drug resistance was also observed in one cat in the GC376 test. Fortunately, none of the other cats in the current study showed signs of drug resistance. However, for future cats that do not respond at all or do not respond well to primary or secondary treatment, this option should be considered.
The initial dose of GS-441524 used in the present study was determined based on previous pharmacokinetic and experimental infectious studies with laboratory cats. These studies indicated that 2.0 and 5.0 mg / kg SC q24h for 14 days would be equally effective in the clinical study. Therefore, a dose of 2.0 mg / kg was chosen for clinical trials, as this would reduce drug consumption by 60%. Although this decision was confirmed in 18/26 cats, eight other cats either suffered relapses (two even twenty) or required a longer duration of treatment to get key blood levels back to normal. Therefore, a decision was made to increase the dose of GS-441524 from 2.0 mg / kg to 4.0 mg kg SC q24h in cats that relapsed or required prolonged treatment. The success rate of 4.0 mg / kg SC q24h in at least 12 such cats, as well as in one cat with a neurological disease, led us to the conclusion that this is a more effective dosage and should become the basis for future treatment.
It was important to monitor simple biological indicators of progress over ⩾ 12 weeks of treatment. HCT (PCV) levels, serum total protein, globulin and albumin levels, and the A: G ratio were identified as useful markers. Based on these parameters, it was shown that the cats had not yet fully recovered after 6-10 weeks of treatment. This finding confirmed the minimum 12-week duration of treatment determined in a previous GC376 clinical trial. Chronic anemia (inflammation anemia) affects 18-95% people with acute and chronic infections and is normocyte / normochromic and unrelated to iron deficiency. Plasma albumin levels were also a good indicator of disease activity, and low albumin and low HCT (PCV) are known to correspond to the incidence of chronic disease. Hyperglobulinemia in cats with FIP has been classified as infectious / inflammatory and is caused by an increase in all classes of gamma globulins and variable increases in the alpha-2 globulin fraction. The marked tendency of cats with FIP to high serum globulin and low albumin levels makes the A: G ratio a particularly good indicator of disease activity.
Purebred cats were not expected to respond as well to treatment due to their genetically impaired ability to respond immunologically to FIPV, and younger cats with wet FIP were expected to respond best to treatment. In this study, however, purebred cats eventually responded as well as regular cats, and the breeds represented by the cats in the study reflected the most popular current breeds. Older cats and cats with pure non-fusion FIP responded to GS-441524 as well as young cats and cats with wet FIP. Assuming that some cats with ocular and neurological diseases can also be treated with GS-441524, it can be said that no more manifestations of FIP may be considered incurable.
The safety profile of GS-441524 was impressive. Based on CBC and serum chemistry, no significant systemic signs of toxicity were observed during the total treatment periods of 12 to 30 weeks, with one possible exception. One cat (CT53) had a slight increase in BUN and SDMA in the 8th week of the third round of treatment and forced treatment to be stopped as a precautionary measure. Based on previous experience with GC376, there have been concerns about the effect of GS-441524 on the development of permanent teeth. Three cats (CT52, CT74, CT77) in this study were 4 months of age or younger and still had juvenile teeth and none showed any subsequent dental abnormalities. Injection site reactions were observed with GS-441524, but their number was remarkably low and easy to treat. It has not been established whether the drug, diluent or both are to blame. Diluent pH 1.5 was well below the FDA (Food and Drug Administration) minimum threshold of 4.5, but drugs of this type are difficult to dissolve and stabilize at a more physiologically acceptable pH. Nevertheless, more physiological diluents should be evaluated.
One cat in the study (CT80) had disturbing clinical signs. Although the cat showed effusive abdominal FIP, it also had long-term symptoms of vague hind limb curvature, low back pain, regular falling episodes, reluctance to jump to higher ground, and unexplained and transient behavioral changes. These symptoms led to the treatment of the cat long after the abdominal effusion disappeared. Finally, a decision was made to discontinue treatment and see if the characteristic symptoms of FIP returned. The cat was eventually euthanized and necropsied that it had a congenital HCM type and no residual FIP or viral RNA lesions in any tissues. Dilated cardiomyopathy has been reported in 17.6% HIV-infected people on chronic antiretroviral therapy. However, it was concluded that GS441524 was not the cause of the heart disease in this cat. Heart disease in this cat was hypertrophic in contrast to the dilatation form observed in HIV patients, and in addition, HCM is relatively common in shelter cats.
Conclusions
The results obtained from 31 cats treated with GS-441524 exceeded all expectations and suggest that FIP, regardless of signaling or disease form, is a treatable disease using nucleoside analogs. The study design and treatment parameters resulting from this limited clinical trial will be important for further efforts in the commercialization of this or similar anti-FIP drugs.
Additional material



Thanks
We thank the staff of the Center for Pet Health for their help in transporting medicines (Lyra Pineda-Nelson and Nancy Bei) and for presenting the data (Cynthia Echeverria). We are especially grateful to the many owners and 31 cats who took part in an emotional and demanding journey that exceeded all expectations. We are also grateful to the practical private veterinarians who helped with the regular blood tests and were there for us and their patients / owners when needed.
Notes
Received: December 28, 2018
Additional material: The following files are available: Client consent form.
Figure S1: Mean liver enzyme levels (IU / l) in cats during GS-441524 treatment. No significant changes were observed throughout the treatment periods.
Figure S2: Mean serum lipase and amylase levels (IU / l) in cats during GS-441524 treatment. No significant changes were observed throughout the treatment periods.
Figure S3: Mean urea and creatinine blood levels in cats during GS-441524 treatment. No significant changes were observed throughout the treatment periods.
Conflict of Interest: MP and EM are employees of Gilead Sciences, Foster City, CA, USA and have stakes in the company.
Funding: Financial support for this study was provided by the UC Davis Center for Animal Health, the Philip Raskin Fund in Kansas City, and numerous SOCK FIP donors as directed by Carol Horace. GS-441524 used in this experiment was provided by Gilead Sciences, Foster City, CA.
References
| 1. | De Clercq, E, Li, G. Approved antiviral drugs over the past 50 years. Clin Microbiol Rev 2016; 29: 695–747. Google Scholar | Crossref | Medline |
| 2. | Hartmann, K. Efficacy of antiviral chemotherapy for retrovirus-infected cats: what does the current literature tell us? J Feline Med Surg 2015; 17: 925–939. Google Scholar | SAGE Journals | ISI |
| 3. | Thomasy, SM, Shull, O, Outerbridge, CA. Oral administration of famciclovir for treatment of spontaneous ocular, respiratory, or dermatologic disease attributed to feline herpesvirus type 1: 59 cases (2006–2013). J Am Vet Med Assoc 2016; 249: 526–538. Google Scholar | Crossref | Medline |
| 4. | Pedersen, NC, Elliott, JB, Glasgow, A. An isolated epizootic of hemorrhagic-like fever in cats caused by a novel and highly virulent strain of feline calicivirus. Vet Microbiol 2000; 73: 281–300. Google Scholar | Crossref | Medline | ISI |
| 5. | Kim, Y, Shivanna, V, Narayanan, S. Broad-spectrum inhibitors against 3C-like proteases of feline coronaviruses and feline caliciviruses. J Virol 2015; 89: 4942–4950. Google Scholar | Crossref | Medline |
| 6. | Pedersen, NC, Kim, Y, Liu, H. Efficacy of a 3C-like protease inhibitor in treating various forms of acquired feline infectious peritonitis. J Feline Med Surg 2018; 20: 378–392. Google Scholar | SAGE Journals | ISI |
| 7. | Pesteanu-Somogyi, LD, Radzai, C, Pressler, BM. Prevalence of feline infectious peritonitis in specific cat breeds. J Feline Med Surg 2006; 8: 1–5. Google Scholar | SAGE Journals | ISI |
| 8. | Riemer, F, Kuehner, KA, Ritz, S. Clinical and laboratory features of cats with feline infectious peritonitis - a retrospective study of 231 confirmed cases (2000–2010). J Feline Med Surg 2016; 18: 348–356. Google Scholar | SAGE Journals | ISI |
| 9. | Rohrbach, BW, Legendre, AM, Baldwin, CA. Epidemiology of feline infectious peritonitis among cats examined at veterinary medical teaching hospitals. J Am Vet Med Assoc 2001; 218: 1111–1115. Google Scholar | Crossref | Medline | ISI |
| 10. | Warren, TK, Jordan, R, Lo, MK. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature 2016; 531: 381–385. Google Scholar | Crossref | Medline | ISI |
| 11. | Sheahan, TP, Sims, AC, Graham, RL. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Transl Med 2017; 9. DOI: 10.1126 / scitranslmed.aal3653. Google Scholar | Crossref |
| 12. | Murphy, BG, Perron, M, Murakami, E. The nucleoside analog GS-441524 strongly inhibits feline infectious peritonitis (FIP) virus in tissue culture and experimental cat infection studies. Vet Microbiol 2018; 219: 226–233. Google Scholar | Crossref | Medline |
| 13. | Takano, T, Endoh, M, Fukatsu, H. The cholesterol transport inhibitor U18666A inhibits type I feline coronavirus infection. Antiviral Res 2017; 145: 96–102. Google Scholar | Crossref | Medline |
| 14. | Takano, T, Nakano, K, Doki, T. Differential effects of viroporin inhibitors against feline infectious peritonitis virus serotypes I and II. Arch Virol 2015; 160: 1163–1170. Google Scholar | Crossref | Medline |
| 15. | Kim, Y, Liu, H, Galasiti Kankanamalage, AC. Reversal of the progression of fatal coronavirus infection in cats by a broad-spectrum coronavirus protease inhibitor. PLoS Pathog 2016; 12: DOI: 10.1371 / journal.ppat.1005531. Google Scholar | Crossref |
| 16. | Gut, M, Leutenegger, CM, Huder, JB. One-tube fluorogenic reverse transcription-polymerase chain reaction for the quantitation of feline coronaviruses. J Virol Methods 1999; 77: 37–46. Google Scholar | Crossref | Medline | ISI |
| 17. | Agostini, ML, Andres, EL, Sims, AC. Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. MBio 2018; 9. DOI: 10.1128 / mBio.00221-18. Google Scholar |
| 18. | Weiss, G, Goodnough, LT. Anemia of chronic disease. N Engl J Med 2005; 352: 1011–1023. Google Scholar | Crossref | Medline | ISI |
| 19. | Kurnick, JE, Ward, HP, Pickett, JC. Mechanism of the anemia of chronic disorders: correlation of hematocrit value with albumin, vitamin B12, transferrin, and iron stores. Arch Intern Med 1972; 130: 323–326. Google Scholar | Crossref | Medline |
| 20. | Taylor, SS, Tappin, SW, Dodkin, SJ. Serum protein electrophoresis in 155 cats. J Feline Med Surg 2010; 12: 643–653. Google Scholar | SAGE Journals | ISI |
| 21. | Hirschberger, J, Hartmann, K, Wilhelm, N. Clinical symptoms and diagnosis of feline infectious peritonitis. Tierarztl Prax 1995; 23: 92–99. Google Scholar | Medline |
| 22. | Pedersen, NC, Liu, H, Gandolfi, B. The influence of age and genetics on natural resistance to experimentally induced feline infectious peritonitis. Vet Immunol Immunopathol 2014; 28: 152–154. Google Scholar |
| 23. | Jain, N, Reddy, DH, Verma, SP. Cardiac abnormalities in HIV-positive patients: results from an observational study in India. J Int Assoc Provid AIDS Care 2014; 13: 40–46. Google Scholar | SAGE Journals |
| 24. | Payne, JR, Brodbelt, DC, Luis Fuentes, V. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centers (the CatScan study). J Vet Cardiol 2015; 17 Suppl 1: S244 – S257. Google Scholar | Crossref | Medline |